Paying It Forward: War, disease, and the science that saves us #138
WHO estimates vaccination prevents 3.5-5 million annual disease deaths, e.g. diptheria, & measles. Vaccinations have eradicated smallpox & polio bype A&B, yet we take medical advice from social media.
Jack Browne, Wichita Falls Times Record News edition, Sunday November 2, 2025
History is often told through the lens of conflict — wars that reshaped borders and ideologies. But alongside these upheavals, another story unfolds: the relentless march of science, especially in medicine.
From the end of the Civil War in 1865 to the COVID-19 pandemic in 2020, each major global disruption has spurred breakthroughs that improved human health and extended lifespans. The relationship between war, disease, and scientific progress is not just coincidental — it’s catalytic.
The 1846 discovery of ether in 1846 before the war revolutionized surgery. After the Civil War ended in 1865, battlefield medicine was forced to evolve. The horrors of infection led to the adoption of antiseptic techniques and the germ theory of disease. These foundational shifts paved the way for modern surgery and public health.
World War I (1915) saw the first widespread use of vaccines to help prevent typhoid among soldiers, and the 1918 flu pandemic pushed nations to invest in epidemiology.
By World War II (1940), penicillin was mass-produced, saving countless lives from bacterial infections. The war also advanced trauma care and blood transfusion techniques, which later became standard in civilian medicine.
In 1965, during the Vietnam War, global health took center stage. The World Health Organization launched aggressive campaigns against smallpox and malaria. Smallpox was eradicated by 1980 — a triumph of international cooperation and scientific rigor.
Wounded soldiers’ survival rates increased significantly with quick triage administered close to the battlefront. These learnings improved treatment of emergency room patients.
The post-9/11 era brought fears of bioterrorism, prompting massive investment in biotechnology. The Human Genome Project, completed in 2003, unlocked new pathways for personalized medicine.
HIV/AIDS research accelerated, turning a fatal diagnosis into a manageable condition. These advances laid the groundwork for rapid-response vaccine platforms that would prove critical in the next global crisis.
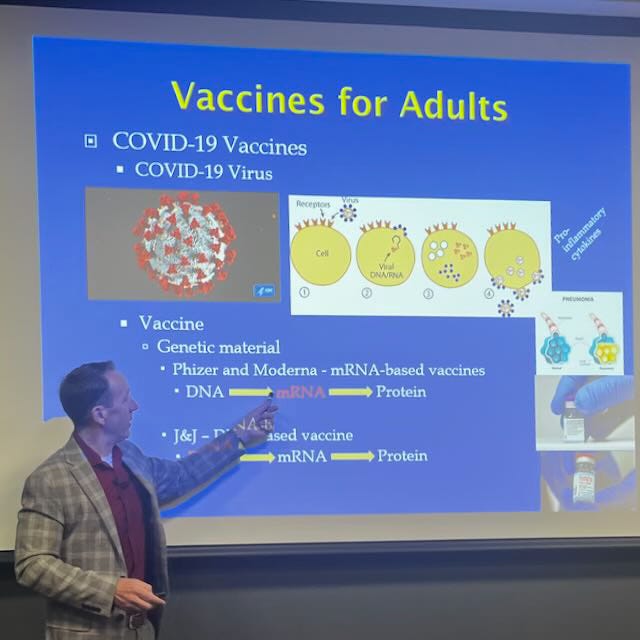
The COVID-19 pandemic was not a war in the traditional sense, but it mobilized the world like one. In less than a year, scientists developed and deployed mRNA vaccines — a technology decades in the making. These vaccines saved an estimated 2.5 million lives globally and added 14.8 million life-years between 2020 and 2024.
Yet, vaccine hesitancy persists. One acquaintance told me, “I’ll get my flu shot, but not a COVID shot. There are over 40 variants of COVID.”
It’s a common refrain, but it misses the mark.
Vaccines still work against variants. While no vaccine is perfect, studies show that COVID vaccines consistently reduce the risk of severe illness, hospitalization, and death — even against newer variants like Delta, Omicron, XBB and this year’s XFG variant — aka “Stratus.”
Flu and COVID are not the same. The flu mutates annually, and we update vaccines accordingly. COVID vaccines have followed a similar path, with boosters tailored to dominant strains. The presence of variants doesn’t negate the value of vaccination—it reinforces it.
The “40 variants” argument is misleading. Yes, SARS-CoV-2 has evolved, but not all variants are equally dangerous. Vaccines target the spike protein, and even with mutations, they still offer protection.
Think of your COVID vaccination like wearing a seatbelt. It may not prevent every injury, but it dramatically improves your odds.
Real-world impact matters. During the Omicron wave, vaccines prevented 57% of potential deaths, mostly among people over 60. That’s not theoretical—that’s millions of families spared grief.
Side effects are rare and manageable. Concerns about myocarditis or blood clots have been studied extensively. The risks are far lower than the dangers of COVID itself, especially for older adults and those with underlying conditions.
Across history, war and disease have forced humanity to innovate. But it’s not just about survival. It’s also about progress. The COVID-19 vaccine wasn’t just a scientific achievement; it was a humanitarian one. It showed what’s possible when urgency meets collaboration.
Today, we live longer and healthier lives because of the lessons learned in times of crisis.
From antiseptics to antibiotics and from genome mapping to mRNA vaccines, science has paid forward the sacrifices of the past.
And as we face future challenges— emerging diseases and aging populations—we must remember that progress is not passive. It’s a choice.
Let’s keep choosing it.
Jack Browne is a community activist and former technology engineer, sales and marketing executive at Motorola and other top tech companies.

